We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
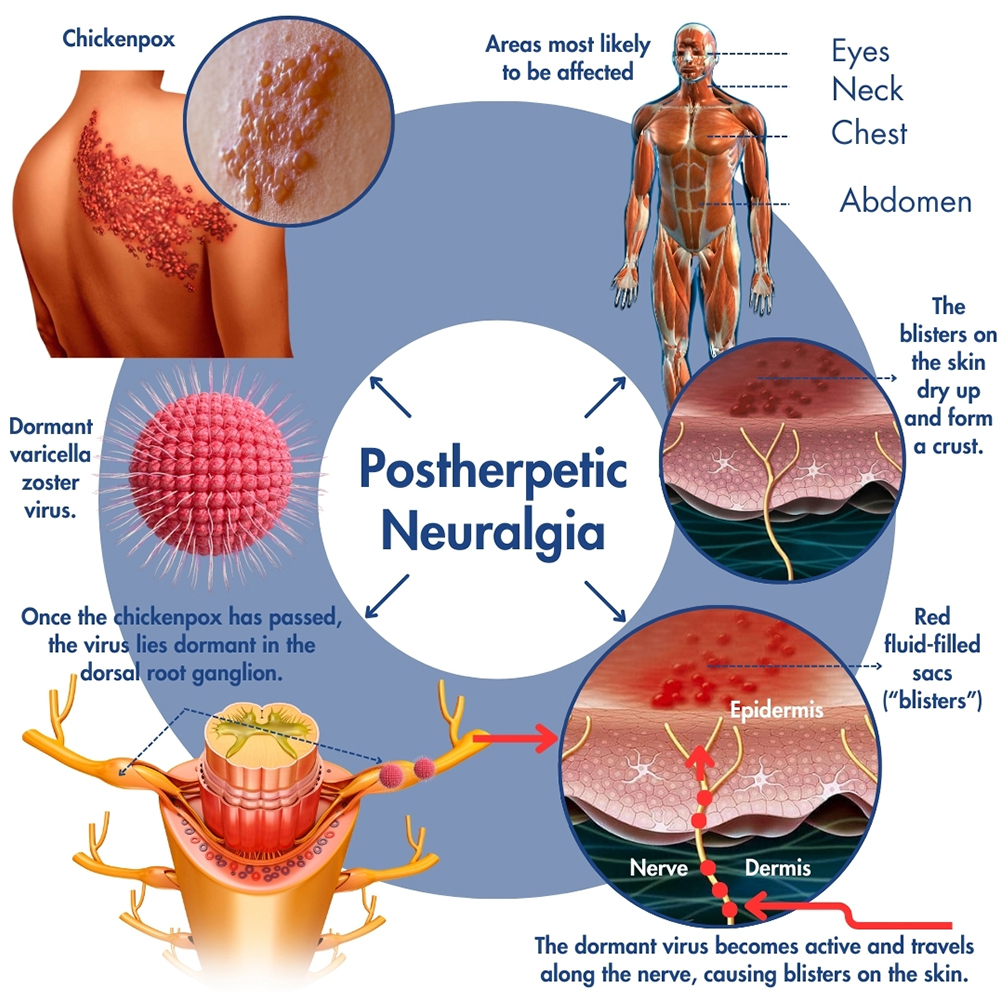 Postherpetic neuralgia (PHN) is a nerve pain complication of shingles. Neuralgia is nerve pain and postherpetic means “after,” as in caused by, the herpes zoster virus that causes shingles. Shingles arise from the reactivation of the varicella-zoster virus (VZV), which is responsible for both shingles and chickenpox (varicella). The initial infection with VZV leads to chickenpox, after which the virus enters a dormant state within the nerve roots of the spine. Therefore, anyone who has had chickenpox is at risk of getting shingles. The chickenpox virus that is dormant in the nerve tissues reactivates and causes a bout of shingles.
Postherpetic neuralgia (PHN) is a nerve pain complication of shingles. Neuralgia is nerve pain and postherpetic means “after,” as in caused by, the herpes zoster virus that causes shingles. Shingles arise from the reactivation of the varicella-zoster virus (VZV), which is responsible for both shingles and chickenpox (varicella). The initial infection with VZV leads to chickenpox, after which the virus enters a dormant state within the nerve roots of the spine. Therefore, anyone who has had chickenpox is at risk of getting shingles. The chickenpox virus that is dormant in the nerve tissues reactivates and causes a bout of shingles.
Shingles typically develop when the immune system is weakened or with age-related decline. PHN, characterized by persistent nerve pain, may occur after the shingles rash has subsided.
Chickenpox, caused by the varicella-zoster virus (VZV), is a common childhood illness characterized by an itchy rash of red bumps across the body. After you recover from the initial infection, the virus remains dormant in the nerve tissues near the brain and spinal cord, granting immunity against future chickenpox infections.
Under certain circumstances, however, such as a weakened immune system or general age-related decline, the VZV may reactivate as herpes zoster, leading to an individually distinct syndrome known as shingles. Shingles typically manifests as an itchy rash confined to one side of the body, accompanied by redness, shooting or stabbing pains, tingling sensations, and the formation of blisters that crust over and dry within a week.
While shingles cannot be cured, prompt medical intervention and pain-relieving treatment when symptoms first appear can mitigate their severity and speed up recovery. Immunization offers preventive measures against shingles, and vaccination is often recommended for people over 60 years old, regardless of prior shingles history. The shingles vaccine reduces the risk of shingles by 51% in this age group and remains effective for approximately 5 years.
Notably, shingles itself is not contagious, but people with active shingles rashes can transmit chickenpox to others—primarily children—through direct physical contact. Understanding the nature of chickenpox and shingles, along with preventive measures like vaccination, is important for managing and reducing the impact of these viral infections on public health.
Occasionally, even after the initial shingles pain and rash have resolved, some individuals continue to feel pain in the affected area. This ongoing discomfort is called postherpetic neuralgia. It is characterized by prolonged nerve pain that lasts more than three months following a shingles outbreak, typically starting as the shingles blisters begin to heal.
The severity of the symptoms can be mitigated by prompt identification and treatment of the herpes zoster. On the other hand, delaying treatment may exacerbate postherpetic neuralgia, with the side effects of prolonged problems with pain and the challenge to manage it. In rare instances, individuals may develop PHN independently of shingles skin eruptions, a condition known as zoster sine herpete.
Timely intervention and comprehensive management strategies are essential for alleviating postherpetic neuralgia symptoms and enhancing the quality of life for people affected by this condition.
PHN usually follows a shingles outbreak and manifests as skin-related issues resulting from nerve damage, including pain, numbness, and itching.
Symptoms of postherpetic neuralgia comprise three distinct types of pain:
The intensity of pain associated with postherpetic neuralgia can vary, ranging from mild discomfort to severe agony, often localized to one side of the body, such as the torso or face. Shingles affecting the facial area may lead to trigeminal neuralgia, which results in long-term facial pain due to inflammation of or damage to the trigeminal facial nerve. Furthermore, in rare cases, individuals may experience muscle weakness or other muscle-related issues if the affected nerves also regulate muscle movement.
Chronic postherpetic neuralgia can be challenging to manage but several treatment options exist, including the following:
The most effective treatment plan often involves a combination of therapies tailored to the individual’s symptoms and needs, and early intervention can significantly improve outcomes.
If you sense the onset of a shingles outbreak, the most effective strategy to minimize or potentially prevent lingering nerve problems is to promptly address the symptoms. It’s crucial to seek medical attention from your healthcare provider as soon as possible. If you are already experiencing shingles, your pain doctor will collaborate with you to effectively manage the symptoms. Early intervention plays a vital role in alleviating discomfort and enhancing recovery, so contact us today for a consultation with one of the pain management experts at Pro Spine & Pain in Wisconsin.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss