We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
While both neuropathy and neuralgia involve nerve damage, they differ in symptoms and causes. Neuropathy encompasses general diseases or dysfunctions of the nerves, while neuralgia involves severe pain that is specific to the path of a damaged nerve and that can be triggered by mild stimulation of the area.
Neuropathy and neuralgia are complex conditions that can have a profound impact on your life. Our team of experienced healthcare professionals at Pro Spine & Pain utilizes various diagnostic tools in the treatment of neuropathy and neuralgia to manage these conditions effectively. Find your neuralgia and neuropathy doctor at one of our five locations throughout Wisconsin.
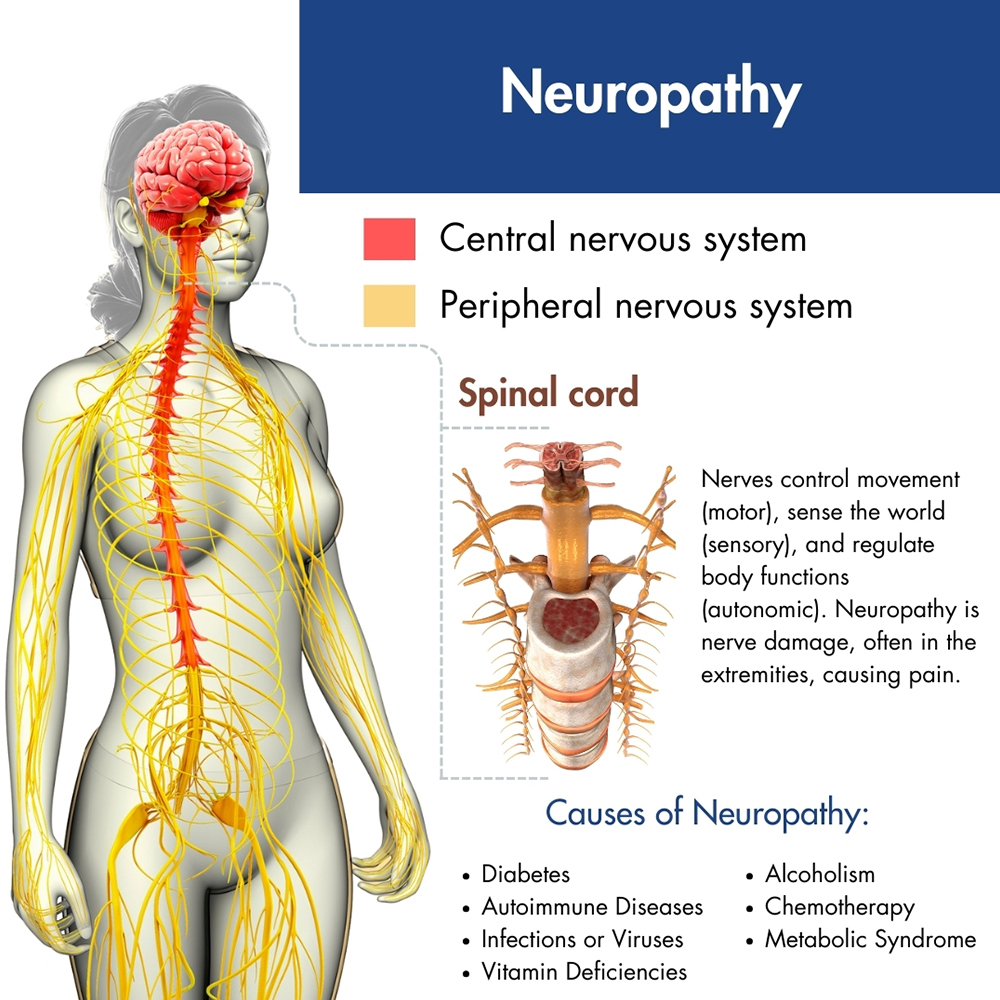 Neuropathy encompasses conditions resulting in nerve damage, leading to symptoms like numbness, including facial numbness, muscle weakness, and nerve pain that can affect daily life. Also known as peripheral neuropathy, it involves the nerves outside the brain and spinal cord, crucial for transmitting information throughout the body. Damage to these nerves can cause various sensations and is progressive without treatment. Early diagnosis and intervention are vital to managing neuropathy effectively and preventing complications. Over 20 million Americans are estimated to have peripheral neuropathy, and it is more common in older individuals.
Neuropathy encompasses conditions resulting in nerve damage, leading to symptoms like numbness, including facial numbness, muscle weakness, and nerve pain that can affect daily life. Also known as peripheral neuropathy, it involves the nerves outside the brain and spinal cord, crucial for transmitting information throughout the body. Damage to these nerves can cause various sensations and is progressive without treatment. Early diagnosis and intervention are vital to managing neuropathy effectively and preventing complications. Over 20 million Americans are estimated to have peripheral neuropathy, and it is more common in older individuals.
Neuropathy can have various causes, and effective pain management is essential for patient recovery.
Common factors contributing to neuropathy include:
Neuropathy affects approximately 20 million people in the United States, with older adults and those with underlying health conditions being the most susceptible demographic.
Risk factors for neuropathy include:
Neuropathy manifests in a variety of symptoms depending on the nerves involved, and nerve function might be subject to change both at the site of nerve damage and within regions of the central nervous system, a condition known as central sensitization.
Early signs may include:
The severity of peripheral neuropathy symptoms varies widely among individuals, ranging from mild numbness or tingling to severe pain, weakness, or interference with daily activities.
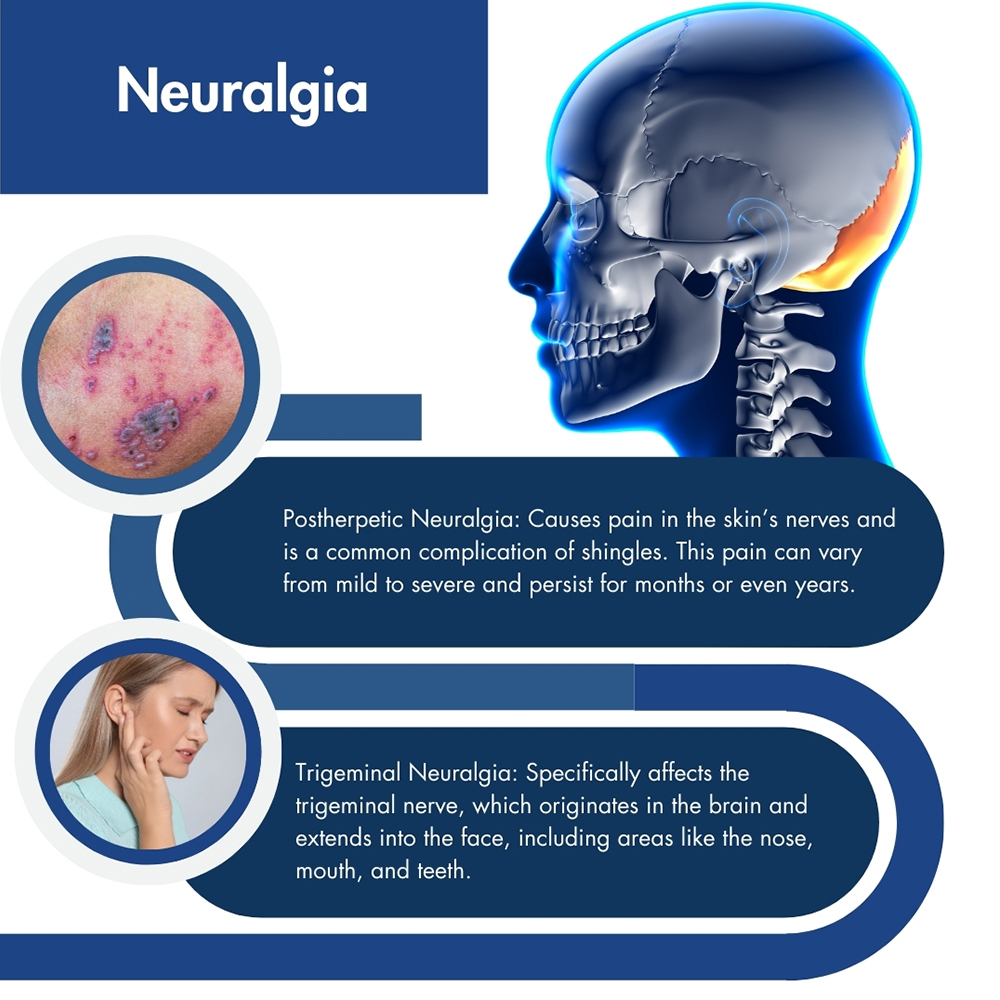 Neuralgia is sharp, shocking pain caused by nerve irritation or damage, significantly affecting quality of life. Trigeminal neuralgia, the most common form, impacts about 12 in every 100,000 people yearly. Neck issues, such as compressed nerves due to spinal misalignment, can trigger trigeminal neuralgia.
Neuralgia is sharp, shocking pain caused by nerve irritation or damage, significantly affecting quality of life. Trigeminal neuralgia, the most common form, impacts about 12 in every 100,000 people yearly. Neck issues, such as compressed nerves due to spinal misalignment, can trigger trigeminal neuralgia.
Neuritis is another condition that is similar to neuralgia. They are related to nervous system conditions, but they differ in nature. Neuralgia involves severe, shock-like pain along nerve paths, while neuritis is nerve inflammation, often leading to symptoms like numbness, weakness, or sensory changes.
There are two main types of neuralgia: postherpetic neuralgia and trigeminal neuralgia.
Various health conditions and external factors can lead to neuralgia.
Common causes include:
The type of people most impacted by neuralgia depends on the type of this condition. For instance, trigeminal neuralgia is more prevalent in individuals over 50, with a higher incidence among women. Postherpetic neuralgia typically affects older adults who have had shingles.
Specific factors to consider include:
Neuralgia manifests as intense, sharp, and often shock-like pain along the pathway of a nerve.
Symptoms may differ depending on the type and severity of neuralgia, but common indicators include:
The severity and frequency of these symptoms vary widely among individuals. While some may experience mild, sporadic pain, others may endure severe and continuous discomfort. Additionally, certain triggers, such as light touch or movement, can provoke pain episodes.
Finding a skilled neuralgia doctor is crucial for effective management and treatment. The pain management specialists at Pro Spine & Pain possess a deep understanding of nerve-related disorders and are proficient in utilizing the latest diagnostic tools and treatment methods.
At Pro Spine & Pain, we take a comprehensive approach to diagnose conditions such as neuropathy and neuralgia. Our diagnostic process will include a full review of your medical history to assess all the details of your symptoms, including details such as onset, intensity, duration, and factors that worsen or alleviate pain. Your physician may also recommend diagnostic imaging such as X-rays, MRI, or CT scans. These tests provide visual insights into affected nerves and surrounding structures, aiding in accurate diagnosis.
In certain cases, there may be nerve conduction studies or electromyography to measure nerve and muscle electrical activity. If applicable, you will be given a diagnostic nerve block via anesthetic injected into specific nerves to assess if they are the pain source. Procedures like facet joint injections, epidural steroid injections, sacroiliac joint injections, and medial branch blocks help pinpoint discomfort causes.
At Pro Spine & Pain, our professional pain management team provide a comprehensive range of treatment for neuropathy and neuralgia tailored to offer effective pain relief.
Please note that the choice of treatment will depend on the specific type of neuropathy or neuralgia you have, its cause, and your overall health condition. A thorough consultation with one of the pain management professionals at our five Wisconsin locations will determine the most appropriate treatment plan.
At Pro Spine & Pain, our dedication lies in delivering thorough and empathetic care to our patients. For treatment for peripheral neuropathy or neuralgia without the need for surgery, contact us today for a personalized treatment philosophy, informed by the latest advancements in research and methodologies.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss