We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
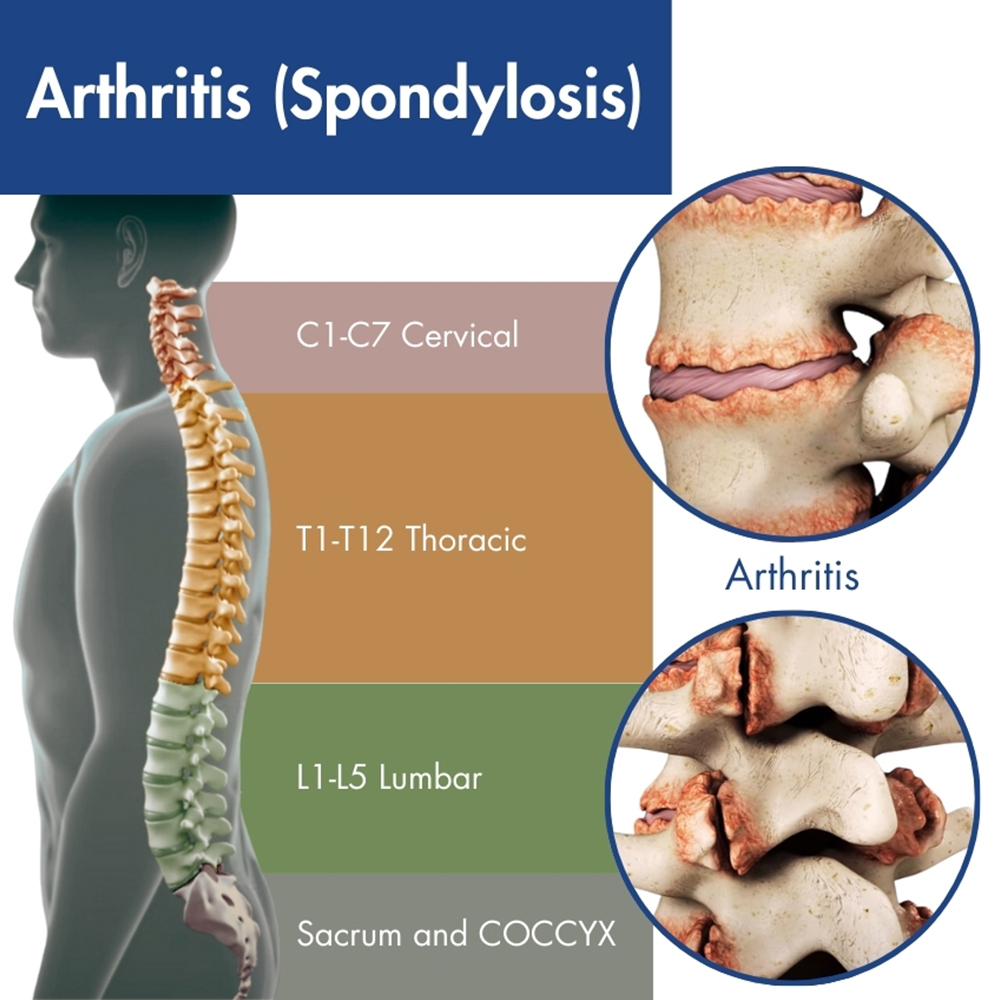 Spondylosis is degenerative arthritis, or osteoarthritis, of the spine, which are the degenerative changes that occur in the spine as a natural part of the aging process. While aging is inevitable, adopting a healthy lifestyle and prioritizing proper back care can mitigate its impact. Seeking expert guidance from your local spine and pain center at the onset of any issues is crucial. Spondylosis, a type of back arthritis, is a degenerative condition that, when addressed promptly, need not limit your mobility. The spine, composed of vertebrae and intervertebral discs, changes over time, including disc degeneration, bone spurs, and other structural alterations.
Spondylosis is degenerative arthritis, or osteoarthritis, of the spine, which are the degenerative changes that occur in the spine as a natural part of the aging process. While aging is inevitable, adopting a healthy lifestyle and prioritizing proper back care can mitigate its impact. Seeking expert guidance from your local spine and pain center at the onset of any issues is crucial. Spondylosis, a type of back arthritis, is a degenerative condition that, when addressed promptly, need not limit your mobility. The spine, composed of vertebrae and intervertebral discs, changes over time, including disc degeneration, bone spurs, and other structural alterations.
Spondylosis treatment often begins with non-surgical approaches, such as working with a physical therapist, medications, and lifestyle modifications. In more severe cases, surgical interventions may be considered to address specific issues like nerve compression or instability in the spine. The goal of treatment is to manage symptoms, improve function, and enhance the overall quality of life for individuals experiencing spondylosis.
If you have back pain spondylosis treatment from Wisconsin’s pain specialists at Pro Spine & Pain can help manage your condition. Contact us to explore your options, with convenient locations in Kenosha, Waukesha, Layton, Franklin, and Madison.
Spondylosis is the natural degeneration of the spine, an inevitable aspect of aging. Your spine consists of 33 vertebrae, extending from the base of your skull to your tailbone. These vertebrae are stacked bones with soft tissue discs in between, facilitating movement, flexibility, and support. With daily use, these discs undergo wear and tear, leading to degeneration over time.
Facet spondylosis refers specifically to the degeneration and inflammation of the facet joints that sit between vertebrae in the spine. It can occur in any region of the spine, but is particularly prevalent in the cervical (neck) and lumbar (lower back) regions.
These changes can lead to symptoms such as pain, stiffness, and reduced flexibility in the affected areas of the spine. Spondylosis is particularly prevalent among individuals over the age of 60, although it can affect people of all ages to varying degrees.
Persistent neck, middle back, or lower back pain unresponsive to self-care warrants evaluation by a spine specialist at a nearby spine pain center. They can diagnose whether spondylosis or another back condition is the culprit. Wisconsin’s leading pain management experts at Pro Spine & Pain specialize in comprehensive treatments for both cervical and lumbar spondylosis. Don’t let unresolved back pain impede your quality of life; seek expert guidance for effective management and relief.
Degenerative disc disease and osteoarthritis are categorized under spondylosis, potentially leading to conditions like spinal stenosis or radiculopathy. Spondylosis manifests in two primary forms: cervical and lumbar. Cervical spondylosis pertains to the neck, encompassing the initial seven vertebrae from the skull’s base. Lumbar spondylosis affects the lower back region, extending around the hip area.
Pain and stiffness are hallmark symptoms of this condition, and these signs can vary in frequency and intensity.
Cervical spondylosis symptoms may include:
Lumbar spondylosis symptoms are similar, but typically affecting the lower body.
Additional symptoms may include:
Understanding these symptoms is crucial for prompt diagnosis and treatment. If you experience any of these signs, consult a healthcare professional for proper evaluation and management. Early intervention can mitigate the problem and improve overall quality of life for individuals affected by spondylosis.
The primary risk factor for developing spondylosis is aging, with individuals over 60 being most susceptible to the condition.
Age-related changes in the back commonly include several factors
These age-related changes highlight the importance of proactive measures to maintain spinal health, such as regular exercise, proper posture, and seeking medical attention for any persistent symptoms or discomfort.
In order to make a diagnosis, your physician will give you a full physical exam, which may include x-rays and a CT scan to pinpoint the areas of degeneration and rule out any other problems.
While aging and spondylosis may be inevitable, their severity can be mitigated through various non-surgical and naturopathic treatments, which are often the initial approach recommended by experienced back pain specialists. Treatment for cervical spondylosis will be the same as for problems in other areas.
Conservative treatments include:
If these methods fail to relieve pain, more advanced treatment options are available, including:
When non-surgical interventions prove insufficient, spine surgery may be considered, especially if spinal cord nerves are affected. Your Wisconsin spine specialist will evaluate your medical history and conduct a thorough physical examination to determine the appropriateness of surgical intervention.
Common spondylosis surgery includes:
For personalized care and treatment options tailored to your needs, contact Pro Spine & Pain in Wisconsin. Their expertise can help address your spondylosis without surgery and determine the most suitable course of action to manage your condition effectively.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss