We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
Your spinal discs resemble small jelly donuts nestled between the vertebrae of your back. Often referred to as intervertebral discs, they are critical structures that serve essential functions contributing to our body’s flexibility, mobility, shock absorption, and overall health. When the soft material inside a disc pushes through the exterior and between the vertebrae, it’s called a herniated disc or slipped disc.
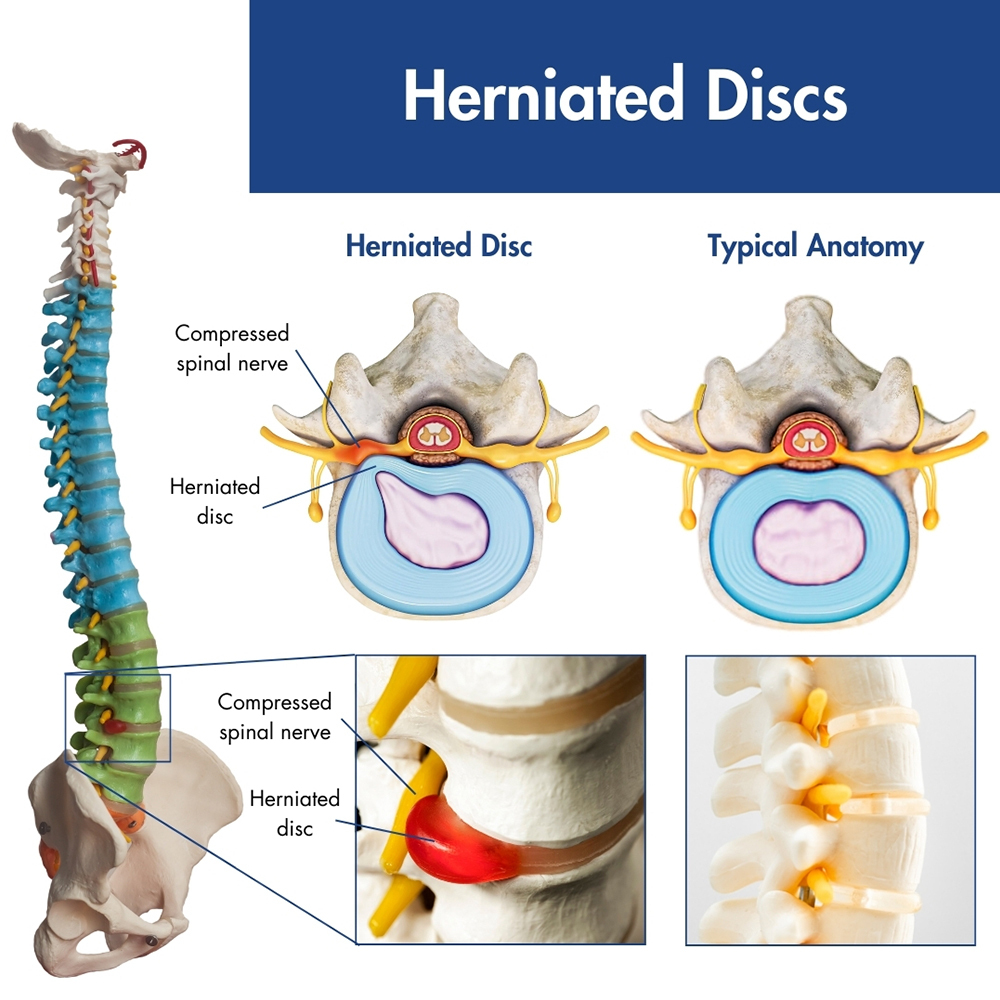
A compromised disc can lead to various scenarios, all of which can cause intense and debilitating pain if it creates pressure on the spinal nerves. For that reason, it’s essential to consult a pain management professional as soon as possible for herniated disc/slipped disc treatment.
Herniated discs can be caused by accident, injury, or just years of continuous wear and tear. Whether you were aware of the incident or not, it is advisable to consult one of our experts at Pro Spine & Pain at the first indication of back pain. Prompt diagnosis and treatment are crucial to prevent further complications or even irreparable nerve damage from a herniated disc. Schedule an appointment now.
Maintaining an active lifestyle exposes your back to considerable stress. Whether engaged in activities like skating, playing tennis, or even routine shopping, your back undergoes significant twisting, turning, bending, and lifting. Irrespective of your fitness level, strenuous activities or repetitive motions can contribute to herniated discs.
If you’re struggling with persistent pain or stiffness in your back or neck, it’s time to seek guidance from the pain management specialists at Pro Spine & Pain who will decide how to treat your herniated disc and create a personalized treatment plan to address any of the acute or chronic pain you may be experiencing.
The lumbar spine—or lower back—is the most commonly affected area when it comes to herniated discs, and lower back pain is a common medical complaint nationwide. If you have a ruptured disc in your lower back, you might experience the following symptoms:
A herniated disc in the neck can also manifest similar symptoms, including:
Certain movements may exacerbate or spread your pain, and prolonged periods in one position can also trigger discomfort. It’s worth noting that you may actually have a herniated disc without noticeable symptoms, and the condition may only be discovered during a routine annual examination.
Nerve roots emerge from the sides of the spinal canal by passing through the small openings located between each vertebra. When a disc herniates or ruptures, it exerts pressure on these nerves, often resulting in a pinched nerve. While you might not pinpoint a specific action causing your back or neck pain, you may recall when the pain first started. It could be associated with using your back muscles to lift a heavy object or making an awkward turn during a physical activity.
For those engaged in athletic or other active pursuits, the risk of back injury, pulled muscles, or herniated discs increases during activities like running, jumping, dancing, or participating in contact sports. Jobs that involve substantial physical demands, including frequent lifting, bending, pushing, or pulling, also pose a risk of back injury . Furthermore, excess body weight can strain the lower back. As you age, the natural aging process may contribute to degenerative joint disease.
While anyone can develop this condition, certain factors increase the risk of experiencing a herniated disc. That means that some people are more likely than others to suffer from this problem.
It is worth mentioning that a variety of non-back-related health conditions can cause pain in the back. Pneumonia or obstructive kidney disease, for example, can result in back discomfort or pain. Hence, when assessing your condition, your back pain specialist in New Jersey should not rule out these processes from the differential diagnosis.
Some of the most distinguishing reasons for back pain are:
Diagnosing herniated disks involves a comprehensive physical and neurological examination, including a full medical history, to assess muscle strength, reflexes, and sensitivity to light touch. To eliminate other potential causes of lower back pain, diagnostic tests such as X-rays, magnetic resonance imaging (MRI), or CT scans may be necessary.
Conservative, nonsurgical treatment will be prioritized by your Wisconsin doctor. If your condition does not respond to these measures, minimally invasive, arthroscopic spine surgery may be considered. A range of treatments may be recommended, progressing from minimally invasive to more intensive:
For expert treatment or surgery for a herniated disc in Wisconsin, reach out to the specialists at Pro Spine & Pain. Schedule an appointment to receive a precise diagnosis and commence appropriate treatment so that you can get back to your daily routines. Our expert pain management physicians specialize in diagnosing and treating back pain.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss