We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
We’re pleased to announce that Pain Physicians of Wisconsin is now Pro Spine Pain.
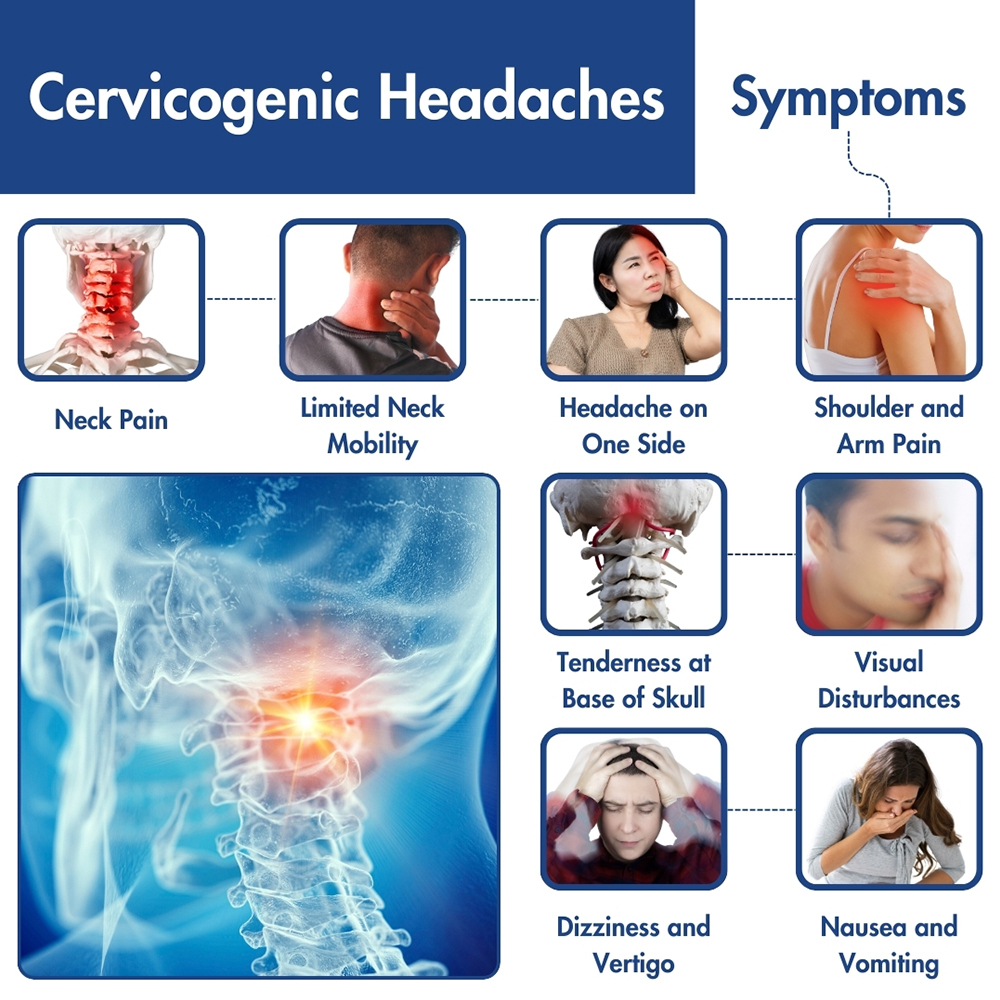 Cervicogenic headaches are a type of severe headache that originates from the cervical spine (neck). Unlike other common types of headaches, like migraines or tension headaches, cervicogenic headaches are often caused by underlying spinal issues in the neck area, inflicting intense pain and impairing the day-to-day life of sufferers. Recognizing the symptoms is crucial for proper diagnosis and effective treatment.
Cervicogenic headaches are a type of severe headache that originates from the cervical spine (neck). Unlike other common types of headaches, like migraines or tension headaches, cervicogenic headaches are often caused by underlying spinal issues in the neck area, inflicting intense pain and impairing the day-to-day life of sufferers. Recognizing the symptoms is crucial for proper diagnosis and effective treatment.
Cervicogenic headaches are a type of secondary headache, because they stem from abnormalities in the bones, nerves, or soft tissues of the cervical region, they can arise from trauma to the head and neck or osteoarthritis of the cervical spine joints, for example.
As medical professionals continue to explore the complex nature of cervicogenic headaches, understanding their connection to spinal pain becomes crucial in developing effective treatment strategies.
The management of this type of headache is very different from that of migraines and tension headaches. For this reason, it’s important to seek a precise diagnosis and comprehensive treatment plan. If you suspect your neck is the culprit behind your headaches, the specialists at Pro Spine & Pain have the expertise to diagnose your condition accurately and provide a fast non-surgical plan for pain relief to get you back to normal.
Cervicogenic headache symptoms can mimic those of a migraine, making the diagnosis difficult. However, there are some differences.
The following conditions are symptomatic of this type of headache:
Diagnosing cervicogenic headaches can be complex and requires a comprehensive approach. Medical professionals typically begin by conducting a thorough medical history review, paying close attention to the patient’s symptoms, including the location, duration, and intensity of the headaches. Physical examinations may focus on assessing neck mobility, muscle tenderness, and any neurological abnormalities. Imaging studies such as X-rays, MRI, CT scans, or electro-diagnosis (EMG) may be ordered to visualize the cervical spine and identify any structural abnormalities or degenerative changes.
Furthermore, diagnostic tests such as nerve blocks or diagnostic injections may be employed to confirm the source of pain by temporarily numbing specific nerves in the neck. This helps differentiate cervicogenic headaches from other types of headaches like migraines or tension headaches. At times, collaborative efforts between neurologists, orthopedic specialists, and pain management experts are often necessary to establish an accurate diagnosis and develop an individualized treatment plan tailored to the patient’s needs and preferences.
Start your journey to a proper diagnosis starts with an experienced pain management doctor, as the type of pain that you may have with cervicogenic headaches can be similar to the symptoms of several types of head or neck disorders. The key to successful treatment is accurately determining the correct source of your pain.
Living with pain caused by cervicogenic headaches is a daily struggle and finding relief can be challenging. The highly skilled pain doctors at Pro Spine & Pain can get right to the source of your pain and provide treatment tailored to your needs. Stop letting pain run your life and request your appointment today.
Treating this problem can involve a multifaceted approach aimed at addressing both the underlying cervical spine issues and managing the associated pain.
Here are some common cervicogenic headache treatment options:
Overall, the treatment approach for cervicogenic headaches will be individualized based on the patient’s specific symptoms, underlying causes, and treatment goals. A multidisciplinary approach involving collaboration between healthcare providers such as neurologists, orthopedic specialists, pain management physicians, physical therapists, and chiropractors may be necessary to optimize outcomes and improve the quality of life for patients.
Thomas Stauss, MD, completed both his undergraduate and medical studies at the esteemed University of Wisconsin in Madison. Dr. Stauss values having access to a wide array of cutting-edge treatment options, ensuring effective relief for his patients' discomfort and a significant enhancement in their quality of life. More specifically, he specializes in utilizing implanted devices to manage chronic pain. Dr. Stauss’s primary objective is to uphold the dignity of each patient while delivering ethical and professional services.
More about Dr. Stauss